Microaggressions and Maternal Health: The Impact on Blood Pressure After Childbirth
A recent study has uncovered a concerning correlation between gender and race-related microaggressions and elevated blood pressure in new mothers, a discovery that has significant implications for maternal health. The research, featured in the Hypertension journal, indicates that over a third of women from Asian, Black, and Hispanic backgrounds experienced racial microaggressions during or post-pregnancy. These subtle, often unintentional, affronts can take the form of dismissive remarks or assumptions that belittle the experiences and identities of minority women, particularly during a critical period in their lives.
The study highlights postpartum hypertension as a significant risk factor, potentially leading to severe health complications, such as heart disease. The connection between racial microaggressions and blood pressure is particularly evident in the postpartum period, especially more than 10 days after giving birth, a time when maternal healthcare often diminishes, leaving many women vulnerable to health issues.
Women who face microaggressions in their prenatal care are more likely to develop persistent hypertension postpartum. This suggests that healthcare providers should extend blood pressure monitoring and hypertension management well beyond the initial postpartum appointment. The study underscores the importance of recognizing that gender and race-based microinsults can trigger physiological stress responses, adversely affecting the health of new mothers.
The research team's analysis of gendered racial microaggressions, in conjunction with blood pressure trends, provides deeper insights into maternal health disparities. Lead researcher Dr. Teresa Janevic points out the prevalence of these microaggressions in healthcare settings, particularly among Black, Hispanic, and South Asian women. Utilizing the Gendered Racial Microaggressions Scale, the study offers a systematic approach to assessing the frequency of these subtle insults, quantifying experiences that were previously only shared anecdotally.
In this research, 373 women were asked to monitor their blood pressure post-childbirth. The results showed that women who reported experiencing microaggressions had significantly higher average systolic and diastolic blood pressure levels than those who did not face such discrimination. Specifically, those who experienced microaggressions had an average blood pressure increase of 2.12 mm Hg and 1.43 mm Hg over three months.
Furthermore, the study found that the association between microaggressions and high blood pressure was particularly strong in areas heavily impacted by structural racism. Women living in these areas exhibited the highest blood pressure levels, highlighting the intersection of systemic issues and personal experiences of discrimination that contribute to increased health risks. These findings raise serious concerns about equitable medical care and the broader social determinants of health affecting minority communities.
Dr. Janevic stresses that the postpartum period, crucial for intervention and health education, has often been overlooked in discussions about new mothers' health management. The study's results indicate an urgent need for healthcare systems to reassess their postpartum support structures, embedding health equity as a core principle in maternal care.
This study serves as a call to action for healthcare practitioners to recognize and address the harmful effects of microaggressions on new mothers. Implementing cultural competency training and educational initiatives may be vital in mitigating biased experiences and fostering more supportive healthcare environments.
Dr. Lisa Levine, the principal investigator of the study, emphasizes the importance of understanding the enduring impacts of racism to enhance equity in maternal healthcare. Strategies for managing hypertension should extend beyond medication to include psychosocial factors that influence health outcomes.
The implications of these findings are far-reaching, suggesting that our understanding of how racism affects the physical health of mothers is still in its early stages. Future research aims to investigate the long-term effects of racism on blood pressure and the overall health of infants born to mothers who experience these disparities during pregnancy and postpartum.
As we move forward, it is essential to continue exploring the link between social disparities and health to uncover interventions that can significantly improve postpartum care. The research indicates a need for a more comprehensive approach, where healthcare systems can proactively tackle obstacles that disproportionately affect marginalized groups and create a healthier environment for all mothers and their children.
Ongoing observation and understanding of postpartum health, especially in relation to racial microaggressions, significantly impact mothers and have lasting effects on families and future generations. In our pursuit of equity in maternal and child health, it is crucial to identify and address the systemic challenges that perpetuate these inequalities
Recent
See All
2025-04-13
Are you potentially susceptible to diabetes? Pay attention to these early warning signs.

2025-04-13
New research has uncovered a critical factor associated with high blood pressure.

2025-04-13
A groundbreaking wellness facility, poised to cater to the needs of individuals overcoming addiction, is scheduled for inauguration in Philadelphia.

2025-04-13
Strategies for Alleviating Cold Sores: Proven Treatments That Work

2025-04-13
In 2025, I've integrated four key exercises into my running regimen to ensure my hips stay robust and injury-free.

2025-04-13
The use of common sleep aids may inadvertently increase the likelihood of Alzheimer's disease.

2025-04-13
<div class="main" data-v-7222d4e3="">

2025-04-13
An Armadale resident, Michael Ashby, has shared his incredible tale of weight loss and improved health.

2025-04-13
A groundbreaking study by a German research team has opened up new possibilities for individuals battling autoimmune diseases.
2025-04-13
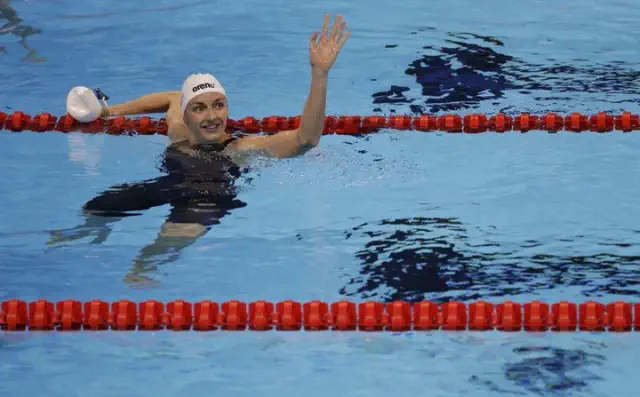
Swimming legend Katinka Hosszu, nicknamed the 'Iron Lady', has announced her retirement after a remarkable career in the sport.
